Women’s Urinary Health and Incontinence
While women may find this topic embarrassing to discuss, it’s important to address.
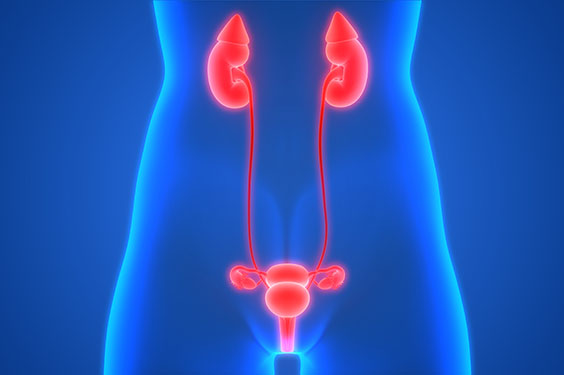
Your urinary system — made up of your kidneys, ureters, bladder and urethra — does several jobs. These include filtering, storing and removing waste from your body. However, millions of women experience urinary incontinence.
Temporary or short-term causes of incontinence include:
- Urinary tract infections (UTIs): An infection inside your urinary tract (urethra, ureters, bladder and kidneys) can cause pain and increase your need to pee more often. Once treated, the urge to urinate frequently usually goes away.
- Pregnancy: During pregnancy, your uterus places extra pressure on the bladder as it expands. Most women who experience incontinence during pregnancy notice that it goes away in the weeks after delivery.
- Medications: Incontinence can be a side effect of certain medications, including diuretics and antidepressants.
- Beverages: There are certain drinks — like coffee and alcohol — that can make you need to urinate much more often. If you stop drinking these beverages, your need to urinate frequently typically goes down.
- Constipation: Chronic constipation (stool that’s hard and dry) can cause you to have bladder control issues.

Chronic or long-term causes of incontinence can include:
- Pelvic floor disorders: When you have an issue with your pelvic floor muscles, it can impact the way your organs function, including your bladder.
- Stroke: A stroke can cause you to experience issues with muscle control. This can include the muscles that control your urinary system.
- Diabetes: When you have diabetes, your body produces more urine. This increase in the amount of urine can cause leakage issues. In addition, peripheral neuropathy can affect the bladder’s function.
- Menopause: Menopause is another time of change in a woman’s body when hormone levels change rapidly and pelvic floor muscles can also become weaker — something that also can happen as you get older.
- Multiple sclerosis (MS): If you have MS, you may experience a loss of control with your bladder, leading to leakage issues.
Types of incontinence
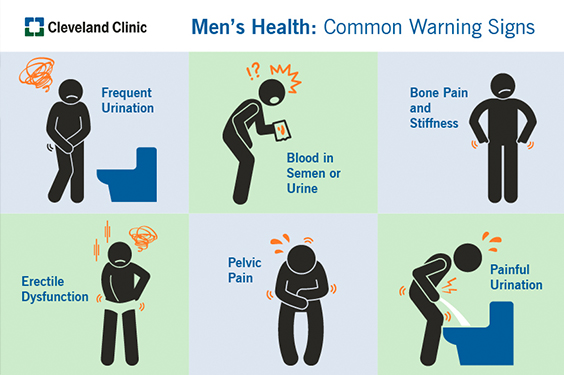
Your men’s urological cancer team
A team-based approach to addressing men’s urological cancer concerns in Medina and the surrounding communities is provided by Dr. Krishnan, along with Michael Gangel, Jr., MD, and John Wegryn, MD.
When to Seek Treatment
If you find that incontinence is disturbing your daily activities and causing you to miss out on things you typically enjoy, you should have a conversation with your primary care or Ob/Gyn physician or a urologist about your medical history and bladder control issues.
“Most people usually mention it to their primary care physician, and will come to a urologist when things aren’t improving or they have bigger symptoms,” says Shannon Wallace, MD, a urogynecologist with Cleveland Clinic’s Ob/Gyn & Women’s Health Institute. Dr. Wallace specializes in pelvic floor disorders and the minimally invasive treatment of stress urinary incontinence, overactive bladder and pelvic organ prolapse. She treats patients at Cleveland Clinic Medina Medical Office Building and main campus.
“Issues like an overactive bladder can be treated with medications, while pelvic floor therapy can address that as well as leakage and mild prolapse.”
Treatment options
There are three main types of treatment for incontinence – medications, lifestyle changes and surgery. Each has pros and cons you should discuss with your provider.
Medications
“Some medications reduce leakage by helping to stabilize muscle contractions that lead to an overactive bladder. Others help relax the bladder to help it empty completely. And hormone replacement therapies — including replacing decreased estrogen during menopause — can help restore bladder function,” says Dr. Wallace.
Lifestyle changes
Lifestyle changes can help improve incontinence. These behaviors include:
- Go to the bathroom on a regular schedule rather than waiting until you feel the urge to go.
- Empty your bladder before physical activity.
- Avoid drinks with caffeine.
- Avoid drinking a lot of fluids before starting an activity or before bedtime.
- Maintain a healthy body weight.
Kegel exercises and pelvic floor therapy, along with use of a vaginal support deceive like a pessary can help strengthen the muscles that you use for holding your urine.
Surgery
“If non-invasive treatment options don’t help, there are surgical options available. For urge incontinence, neuromodulation or interstim therapy consists of a pacemaker-like unit that sends a constant signal to the nerves of the bladder to help it settle down,” says Dr. Bologna. “And for stress incontinence, a small vaginal incision is made to place a sling under the urethra to provide support to stop leakage.”
Therapy
If you’ve been told that you could benefit from pelvic floor therapy, Cleveland Clinic Brunswick Family Health Center has physical therapists who specialize in this treatment.
Roy Miler, MD
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore e.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et
Dolore magna aliqua. Quis ipsum suspendisse ultrices gravida. Risus commodo viverra maecenas accumsan lacus vel facilisis. Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Interested in learning more about Integrative and Lifestyle Medicine?
Medical referrals aren’t necessary and virtual appointments are available for many services offered through Integrative and Lifestyle Medicine. Most insurance companies cover Integrative and Lifestyle Medicine care, but check with your provider about your coverage.
The safety of our patients and caregivers remains our top priority. We want to assure our patients that our Cleveland Clinic facilities are safe for them to receive care. We have taken several steps to increase safety including limiting visitors to our facilities and screening everyone for potential COVID-19 symptoms.
To schedule an appointment with Dr. Bologna or Dr. Wallace in Medina, call 330.721.5700.
For pelvic floor therapy appointments at Brunswick Family Health Center, call 330.225.8886.