From your simplest questions to greatest concerns, Cleveland Clinic men’s health experts are here for every care in the world.
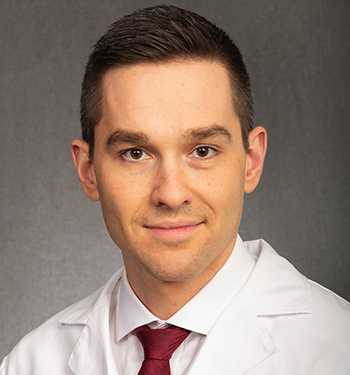
It’s no secret: men are statistically much less likely than women to seek medical care. It’s important for men to consult with their physician if they suspect something is not quite right, but our experts also recommend seeing a urologist regularly, beginning at age 40.
Why Men Over 40 Should Start Seeing a Urologist Regularly
If you’re a man 40 or older, seeing a urologist regularly is most likely the last thing on your mind when you have a million other things to take care of. But as you go through your 40s, quality-of-life issues become more important. A men’s health expert can help guide you on what to expect, useful lifestyle changes, when to simply observe and when to treat a problem.
Men’s health conditions often share the same signs and symptoms. Although there may be a simple explanation and an easy fix, there’s a chance that you could need treatment before something gets worse.
See your doctor whenever you have:
- Blood in your urine or semen.
- Urination problems, including pain or burning, needing to go all the time, difficulty getting started or a weak flow.
- New or worsening erectile dysfunction.
- Painful ejaculation.
- Changes or pain in your testicles or penis, including swelling, hardness, a lump or feeling of heaviness.
- Ongoing pain or stiffness in your lower back, hips or legs.
Men's Health Care Goes Beyond Once-in-a-Lifetime Procedures
Coping with COVID-19
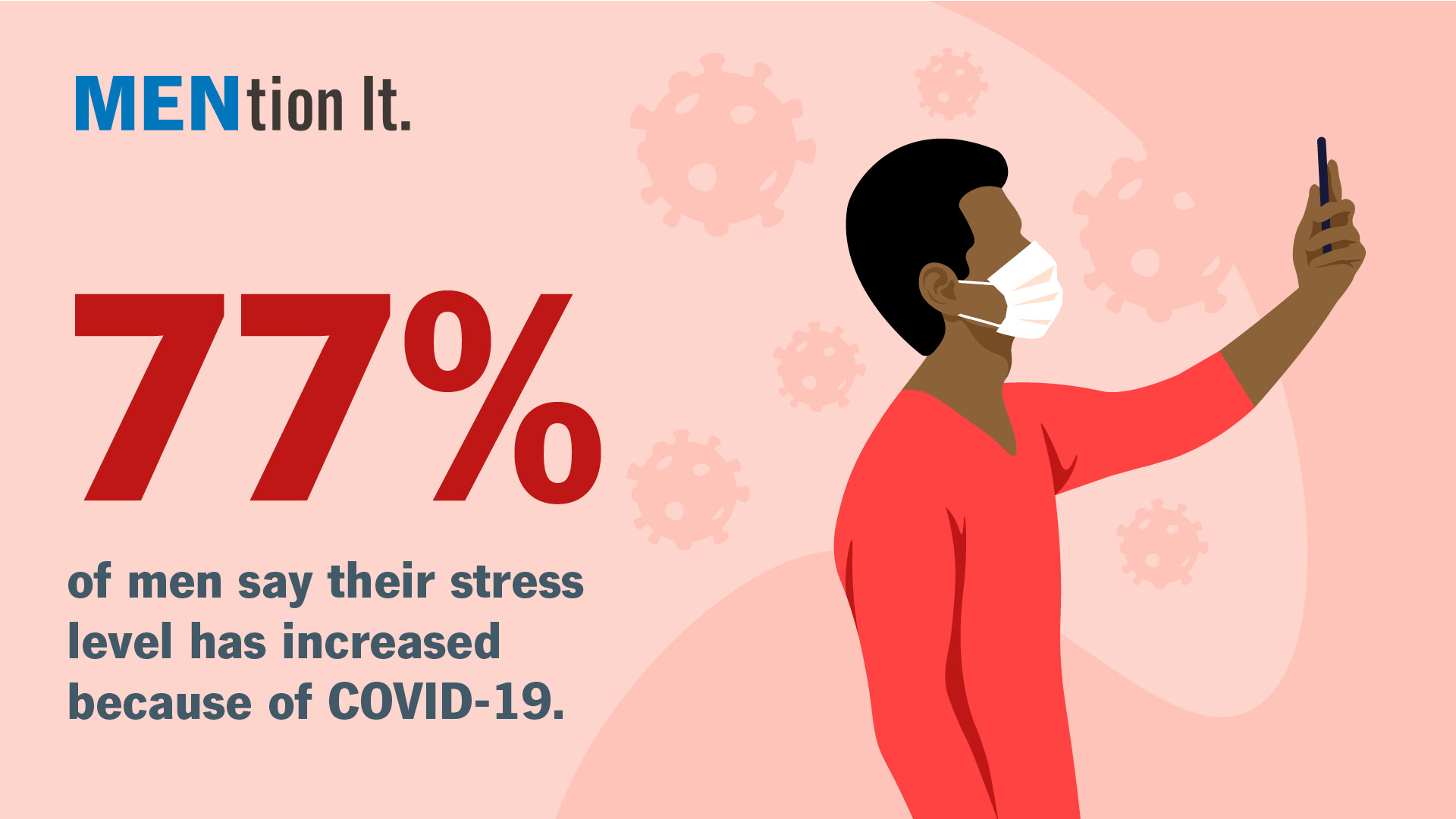
Survey Illustrates the Mental and Physical Toll the Pandemic is Taking on Men
In an online survey among approximately 1,000 U.S. males 18 years or older, Cleveland Clinic found that 77 percent of men report their stress level has increased as a result of COVID-19. Half of men (48%) have put off seeing a doctor for non-COVID-19 related health issues over the last few months – this is even higher among men 18-34 (56%).
“We want to remind men that their health shouldn’t take a back seat, especially during a pandemic,” said Eric Klein, M.D., chairman of Cleveland Clinic’s Glickman Urological & Kidney Institute. “If you’re experiencing symptoms that indicate a real health issue, don’t be afraid to come to the hospital or schedule an appointment with a healthcare provider, either virtually or in person. Your health is too important not to.”
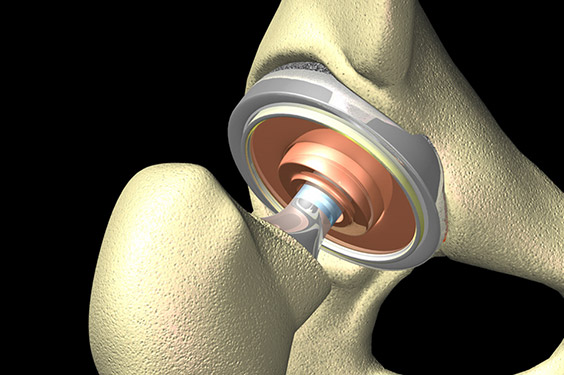
Implant for Total Hip Replacement
New technology
There have been many advancements in joint replacement procedures since they were first performed in the 1960s. Recent advances include:
- Computer “navigation” during surgery allows surgeons to be more precise in placing implants. The more precisely placed an implant is, the better it fits and works.
- Patient-specific instrumentation uses CT or MRI scans of the joint to get 3-D images, aiding the surgeon in knowing exactly where to make a cut.
- Robotic-assisted surgery uses pre-operative imaging and intra-operative navigation with robotic assistance to help preserve joint tissue and enhance the accuracy of implant placement.
Improvements in the use of pain medication
“While it’s unrealistic to expect no pain after surgery, the use of spinal anesthetics, long-acting local anesthetics and regional pain blocks help pinpoint and control pain, keeping postoperative pain on the low end of the scale,” says Dr. Sziraky. “This approach, called multimodal anesthesia, helps hit the pain from different angles, and helps avoid the use of narcotics, which have more side effects.”
Most patients receive a spinal injection that numbs them from the waist down for a couple of hours, along with a long-lasting local anesthetic that helps control pain for up to two days afterward. There is no need for a pain pump for self-administered medications or IV pain killers.
Shorter hospital stays
Typically, joint replacement patients are out of bed and walking the afternoon after surgery, followed by another physical therapy session the next morning. Most go home the day after surgery, with follow-up care at home by a visiting nurse, virtual visits, and occupational and physical therapy.
“Leaving the hospital means you get to recuperate in the comfort of your own home. You’ll progress better in a familiar environment where you’re more likely to get a good night’s sleep,” says Dr. Sziraky.
Durability
Replacement joints today allow for improved motion, and they are lighter and stronger. Hip replacements last on average about 15 years, and approximately 85% of knee implants will last 20 years. Improvements in surgical techniques, prosthetic designs, bearing surfaces, and fixation methods may allow these implants to last even longer.
“With improved implant technology, younger patients have less risk of needing repeat surgeries due to parts wearing out,” Dr. Sziraky adds.
Lorem ipsum dolor sit amet, consectetur adipiscing elit
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore.
Risus commodo viverra maecenas accumsan lacus vel facilisis. Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua.
Prostate, bladder, kidney and testicular cancer
Even minor symptoms that you only notice once can be the sign of something serious. If a simple visit to the bathroom has you seeing red, don’t ignore it. “When you see blood in your urine – whether it’s slightly pink, brown or bright red – get to your doctor within a week or two after you first see it. If it’s cancer, a delay in treatment greatly compromises the cure rate. Though blood in the urine most often comes from a benign condition like kidney stones, enlarged prostate or a urinary tract infection, it also can signal bladder or kidney cancer.” says Robert Abouassaly, MD, a Cleveland Clinic urologist who sees patients at Cleveland Clinic Fairview Hospital.
Prostate cancer is the most common cancer in men and is silent in its early stages. For most, the cancer grows very slowly. You can live with early prostate cancer for years without developing symptoms. Symptoms – such as trouble urinating or feeling like you always need to urinate, particularly at night – start later.
While not as common, testicular cancer also is one of the top cancers in men. Again, the earlier you get care, the better. Testicular cancer is curable in 95% of cases – 98% if treated early.
Nullam in enim ullamcorper, efficitur dui a, fermentum erat. Cras in massa eget nisi imperdiet hendrerit vel interdum tellus. Ut pellentesque neque ipsum, quis fringilla nisl volutpat vel. Cras et luctus ipsum, quis blandit ligula. Morbi elementum tincidunt nibh eu lobortis. Ut consectetur ut libero sed sagittis.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et
Dolore magna aliqua. Quis ipsum suspendisse ultrices gravida. Risus commodo viverra maecenas accumsan lacus vel facilisis. Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Yes, it’s safe to see your doctor again
COVID-19 changed a lot about how you live, including how you go to the doctor. In the early weeks of the pandemic, you may have tried to stay home as much as possible. Your appointments may have been cancelled.
Although COVID-19 is still around and still contagious, Cleveland Clinic has taken steps to allow you to return safely for men’s health and urology care. Safely get the care you need at a Cleveland Clinic location near you.
To protect you, Cleveland Clinic continues to:
- Practice physical distancing and limit the number of people in one area.
- Screen everyone for COVID-19 symptoms.
- Require a face mask for everyone at all Cleveland Clinic locations.
- Disinfect surfaces frequently.
- Encourage virtual visits, when appropriate, to minimize in-person visits.
Connect with Cleveland Clinic now
Need urology care at Cleveland Clinic?
- See a urologist now with Express Care® Online.
- Message your doctor through MyChart.
- Schedule a virtual visit.
- Request an appointment.
- Call 216.444.5600 to schedule an appointment.