Chronic pelvic pain? You’re not alone.
Chronic pelvic pain is fairly common, affecting about one in seven women. About 30% of those women will seek treatment for the pain from their primary care or Ob/Gyn physician.
“Chronic pelvic pain is defined as pain in the lower abdomen, pelvis or genital area that lasts longer than six months,” says Cara King, DO, a Cleveland Clinic Ob/Gyn physician and surgeon who specializes in minimally invasive gynecologic surgery. Dr. King treats patients at Cleveland Clinic Hillcrest Hospital and main campus. “For many women, the pain can be traced to the reproductive organs, but it can also come from the bladder, the gastrointestinal system, or nerves of pelvic and abdominal muscles. In some cases, the pain comes from multiple causes, making it difficult to diagnose the exact cause.”
“The journey to a successful pregnancy has many steps. It starts with being healthy before pregnancy. Maintaining a healthy weight, eating a healthy diet and taking part in regular physical activity may all increase your chances for conception, a healthy pregnancy, less complications during delivery, and most importantly having a healthy baby,” says Jacqueline Zuponcic, DO, an Ob/Gyn at Cleveland Clinic Akron General.
The American College of Obstetricians and Gynecologists (ACOG) also recommends a “preconception counseling” appointment for women who are ready to begin attempting pregnancy. At this appointment, we review your medical history, medications, and risks that you may have — all to help optimize your chances for a healthy new pregnancy.
If you don’t already have a provider, it’s important to choose one you are comfortable with. The team at Akron General includes board-certified obstetrician/gynecologists and advanced practice nurses, as well as maternal-fetal medicine specialists and anesthesiologists who are available 24/7.
“It’s important to begin prenatal care early, with your first visit about eight weeks into your pregnancy, and monthly prenatal visits until around 28 weeks,” says Dr. Zuponcic. “As your due date approaches, you will have more frequent visits so we can closely monitor your health and that of your baby.”
Regular prenatal visits are essential to help you and your baby stay well, to manage any conditions or complications that may arise, and to discuss any questions or concerns you may have along the way.
During pregnancy, testing helps ensure the health of both mom and baby. Akron General offers state-of-the-art ultrasound technology and specialized testing such as amniocentesis, RH sensitization and percutaneous umbilical sampling, and now access to fetal echocardiogram services onsite from Cleveland Clinic Children’s pediatric cardiologists.
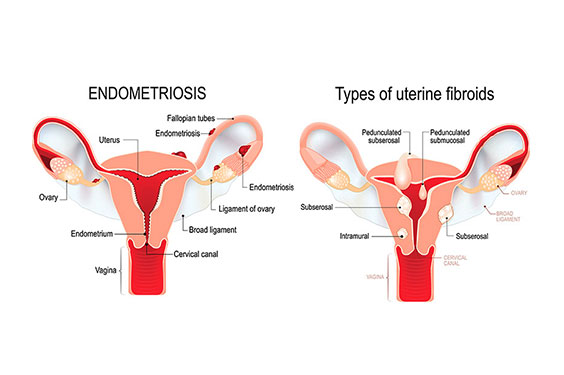
Endometriosis and fibroids are among the many possible causes of chronic pelvic pain.
"If you experience pain during your period, during bowel movements, when urinating, or during intercourse, you should see your primary care doctor or gynecologist,” says Dr. King. “When it comes to diagnosis and treatment, we start with the least invasive options first. In many cases, medication or hormonal therapy — specifically, the use of birth control — that stop or decrease menstrual flow can help.”

Specialized care for high-risk moms and babies
Sometimes, extra care is needed. Akron General cares for mom and baby during high-risk pregnancies and for fragile newborns.
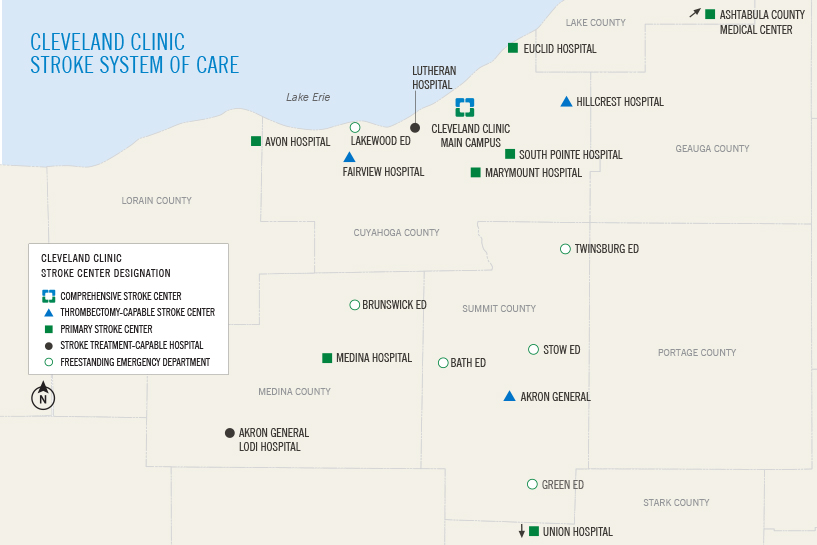
Cleveland Clinic’s stroke system offers high quality care across Northeast Ohio.
Cleveland Clinic cares for one of the largest populations of stroke patients in the country, with more than 6,800 encounters annually. These volumes have allowed us to build one of the best-developed stroke systems of care in the U.S.
Roy Miler, MD
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore e.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et
Dolore magna aliqua. Quis ipsum suspendisse ultrices gravida. Risus commodo viverra maecenas accumsan lacus vel facilisis. Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Roy Miler, MD
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore e.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et
Dolore magna aliqua. Quis ipsum suspendisse ultrices gravida. Risus commodo viverra maecenas accumsan lacus vel facilisis. Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Nullam in enim ullamcorper, efficitur dui a, fermentum erat. Cras in massa eget nisi imperdiet hendrerit vel interdum tellus. Ut pellentesque neque ipsum, quis fringilla nisl volutpat vel. Cras et luctus ipsum, quis blandit ligula. Morbi elementum tincidunt nibh eu lobortis. Ut consectetur ut libero sed sagittis.
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et
Dolore magna aliqua. Quis ipsum suspendisse ultrices gravida. Risus commodo viverra maecenas accumsan lacus vel facilisis. Lorem ipsum dolor sit amet, consectetur adipiscing elit.
To schedule an appointment with Dr. King or another Women’s Health specialist, visit ClevelandClinic.org/WomensHealth or call 216.444.6601.